Near-Infrared Visual Differentiation in Normal and Abnormal Breast Using Hemoglobin Concentrations
Journal of Lasers in Medical Sciences,
Vol. 9 No. 1 (2018),
31 December 2017
,
Page 50-57
Abstract
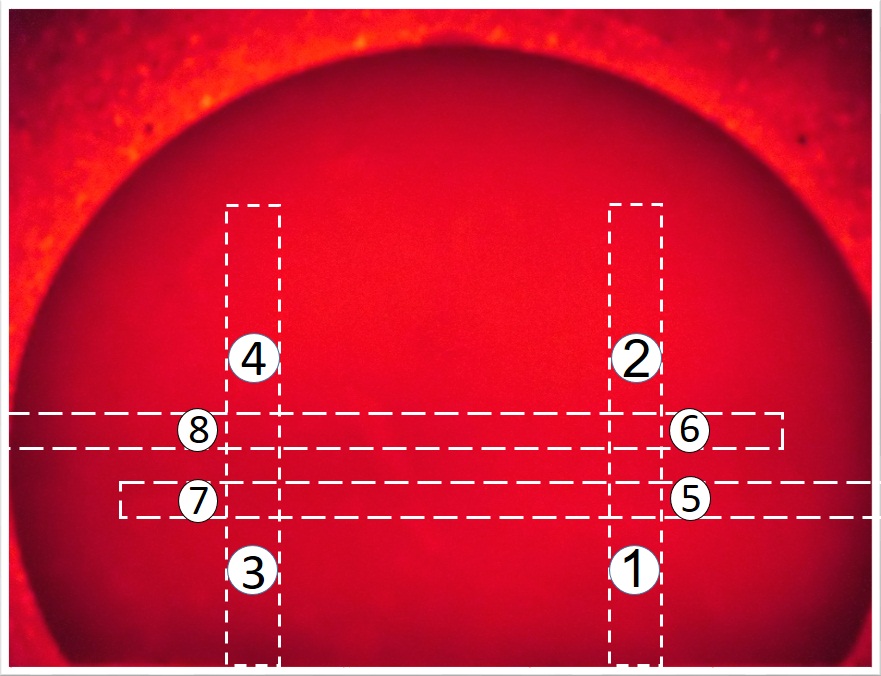
Introduction: Near-infrared (NIR) optical imaging is a non-ionizing modality that is emerging as a diagnostic/prognostic tool for breast cancer according to NIR differentiation of hemoglobin (Hb)concentration.Methods: The transmission values of LED-sourced light at 625 nm were measured by power meter to evaluate the optical properties of Hb in breast phantom containing major and minor vessels. For the simulation of blood variations in cancerous breast condition, we prepared 2 concentrations of pre-menopausal Hb and 4 concentrations of post-menopausal Hb and, for comparison with normal tissue, one concentration of Hb injected inside the phantom’s vessels. Imaging procedure on the phantom was also conducted by LED source and CCD camera. The images from the experiments were compared with the results obtained from the images analyzed by MATLAB software. Finally, mammography of phantom including various concentration of Hb was prepared.
Results: The transmitting intensities of NIR in blood containing 1, 2 and 4 concentrations of Hb in the major vessels were 52.83 ± 2.85, 43.00 ± 3.11 and 31.17 ± 2.27 μW, respectively, and in minor vessels containing similar Hb concentrations were 73.50 ± 2.43, 60.08 ± 5.09 and 42.42 ± 4.86 μW, respectively. The gray-scale levels on the major vessel were about 96, 124, 162 and on the minor vessel about 72, 100, 130 measured for 1, 2 and 4 Hb concentrations, respectively. The sensitivity and specificity of NIR imaging differentiation were 97.4% and 91.3%, respectively.
Conclusion: Significant differences in transmitting intensity, optical imaging as well as software analysis of images were observed for 1, 2 and 4 concentrations of Hb in major and minor breast phantom vessels. Differentiation capability of minor vessels was higher than major vessels for Hb concentrations. Despite a good detection for location of vessels by mammography, it could not show differences between vessels with various concentrations. However, NIR optical imaging demonstrated a good image contrast for showing vessels in terms of concentration. This study recommends NIR optical imaging for prescreening breast cancer due to its potential for early diagnosis.
- Hemoglobin concentrations
- Imaging
- Near-infrared
- Optical properties.
How to Cite
References
Siegel RL, Miller KD, Jemal A. Cancer statistics, 2015. CA Cancer J Clin. 2015;65(1):5-29. doi:10.3322/caac.21254
Godavarty A, Rodriguez S, Jung YJ, Gonzalez S. Optical imaging for breast cancer prescreening. Breast Cancer (Dove Med Press). 2015;7:193-209. doi:10.2147/bctt.s51702
Gautherie M. Thermopathology of breast cancer: measurement and analysis of in vivo temperature and blood flow. Ann N Y Acad Sci. 1980;335:383-415.
Mehnati P, Tirtash MJ. Comparative Efficacy of Four Imaging Instruments for Breast Cancer Screening. Asian Pac J Cancer Prev. 2015;16(15):6177-6186.
Warner E, Plewes DB, Shumak RS, et al. Comparison of breast magnetic resonance imaging, mammography, and ultrasound for surveillance of women at high risk for hereditary breast cancer. J Clin Oncol. 2001;19(15):3524- 3531. doi:10.1200/jco.2001.19.15.3524
Byrne C, Schairer C, Wolfe J, et al. Mammographic features and breast cancer risk: effects with time, age, and menopause status. J Natl Cancer Inst. 1995;87(21):1622- 1629.
van Gils CH, Otten JD, Hendriks JH, Holland R, Straatman H, Verbeek AL. High mammographic breast density and its implications for the early detection of breast cancer. J Med Screen. 1999;6(4):200-204. doi:10.1136/jms.6.4.200
Simick MK, Jong R, Wilson B, Lilge L. Non-ionizing near-infrared radiation transillumination spectroscopy for breast tissue density and assessment of breast cancer risk. J Biomed Opt. 2004;9(4):794-803. doi:10.1117/1.1758269
EtehadTavakol M, Sadri S, Ng EY. Application of K- and fuzzy c-means for color segmentation of thermal infrared breast images. J Med Syst. 2010;34(1):35-42.
Hall EJ, Giaccia AJ. Radiobiology for the Radiologist. Lippincott Williams & Wilkins; 2006.
Wan S, Parrish JA, Anderson RR, Madden M. Transmittance of nonionizing radiation in human tissues. Photochem Photobiol. 1981;34(6):679-681.
Erfanzadeh M, Alikhani S, Ansari MA, Mohajerani E. A low-cost method for optical tomography. J Lasers Med Sci. 2011;3(3):102-108.
Afsari Golshan M, Ghasemi Tarei M, Ansari MA, Amjadi A. The Propagation of Laser Light in Skin by Monte Carlo-Diffusion Method: A Fast and Accurate Method to Simulate Photon Migration in Biological Tissues. J Lasers Med Sci. 2011;2(3):109-114.
Jacques SL. Optical properties of biological tissues: a review. Phys Med Biol. 2013;58(11):R37-61. doi:10.1088/0031- 9155/58/11/r37
Venisnik KM, Olafsen T, Loening AM, Iyer M, Gambhir SS, Wu AM. Bifunctional antibody-Renilla luciferase fusion protein for in vivo optical detection of tumors. Protein Eng Des Sel. 2006;19(10):453-460. doi:10.1093/protein/gzl030
Chen ZY, Wang YX, Lin Y, et al. Advance of molecular imaging technology and targeted imaging agent in imaging and therapy. BioMed Res Int. 2014;2014:12. doi:10.1155/2014/819324
Taber KH, Hillman EM, Hurley RA. Optical imaging: a new window to the adult brain. J Neuropsychiatry Clin Neurosci. 2010;22(4):iv, 357-360. doi:10.1176/appi. neuropsych.22.4.iv
Anderson PG, Kainerstorfer JM, Sassaroli A, et al. Broadband optical mammography: chromophore concentration and hemoglobin saturation contrast in breast cancer. PLoS One. 2015;10(3):e0117322. doi:10.1371/ journal.pone.0117322
Leff DR, Warren OJ, Enfield LC, et al. Diffuse optical imaging of the healthy and diseased breast: a systematic review. Breast Cancer Res Treat. 2008;108(1):9-22. doi:10.1007/s10549-007-9582-z
van Veen RL, Sterenborg HJ, Marinelli AW, Menke- Pluymers M. Intraoperatively assessed optical properties of malignant and healthy breast tissue used to determine the optimum wavelength of contrast for optical mammography. J Biomed Opt. 2004;9(6):1129-1136. doi:10.1117/1.1803547
Etehadtavakol M, Lucas C, Sadri S, Ng EY. Analysis of breast thermography using fractal dimension to establish possible difference between malignant and benign patterns. J Healthc Eng. 2010;1(1):27-43.
Chance B, Nioka S, Zhang J, et al. Breast cancer detection based on incremental biochemical and physiological properties of breast cancers: a six-year, two-site study. Acad Radiol. 2005;12(8):925-933. doi:10.1016/j.acra.2005.04.016
Beaney RP, Lammertsma AA, Jones T, McKenzie CG, Halnan KE. Positron emission tomography for in-vivo measurement of regional blood flow, oxygen utilisation, and blood volume in patients with breast carcinoma. Lancet. 1984;1(8369):131-134.
Andres AC, Djonov V. The mammary gland vasculature revisited. J Mammary Gland Biol Neoplasia. 2010;15(3):319- 328. doi:10.1007/s10911-010-9186-9
Fantini S, Franceschini MA, Gaida G, et al. Frequency-domain optical mammography: edge effect corrections. Med Phys. 1996;23(1):149-157. doi:10.1118/1.597696
Gonzalez J, Roman M, Erickson SJ, Godavarty A. Near- Infrared Hand-Held Optical Imaging Technology. J Indian Inst Sci. 2013;93(1):1-14.
Zhu Q, Cronin EB, Currier AA, et al. Benign versus malignant breast masses: optical differentiation with US-guided optical imaging reconstruction. Radiology. 2005;237(1):57-66. doi:10.1148/radiol.2371041236
Taroni P, Pifferi A, Torricelli A, Spinelli L, Danesini GM, Cubeddu R. Do shorter wavelengths improve contrast in optical mammography? Phys Med Biol. 2004;49(7):1203- 1215.
Spinelli L, Torricelli A, Pifferi A, Taroni P, Danesini G, Cubeddu R. Characterization of female breast lesions from multi-wavelength time-resolved optical mammography. Phys Med Biol. 2005;50(11):2489-2502. doi:10.1088/0031- 9155/50/11/004
van de Ven S, Elias S, Wiethoff A, et al. Diffuse optical tomography of the breast: initial validation in benign cysts. Mol Imaging Biol. 2009;11(2):64-70. doi:10.1007/s11307- 008-0176-x
Cerussi AE, Berger AJ, Bevilacqua F, et al. Sources of absorption and scattering contrast for near-infrared optical mammography. Acad Radiol. 2001;8(3):211-218. doi:10.1016/s1076-6332(03)80529-9
Mehnati P, Jafari Tirtash M, Zakerhamidi MS, Mehnati P. Assessing Absorption Coefficient of Hemoglobin in the Breast Phantom Using Near-Infrared Spectroscopy. Iran J Radiol. 2016;13(4):e31581. doi:10.5812/iranjradiol.31581
Ansari MA, Erfanzadeh M, Hosseini Z, Mohajerani E. Diffuse optical tomography: image reconstruction and verification. J Lasers Med Sci. 2014;5(1):13-18.
Busch DR, Guo W, Choe R, et al. Computer aided automatic detection of malignant lesions in diffuse optical mammography. Med Phys. 2010;37(4):1840-1849. doi:10.1118/1.3314075
Labib NA, Ghobashi MM, Moneer MM, Helal MH, Abdalgaleel SA. Evaluation of BreastLight as a tool for early detection of breast lesions among females attending National Cancer Institute, Cairo University. Asian Pac J Cancer Prev. 2013;14(8):4647-4650.
- Abstract Viewed: 759 times
- PDF Downloaded: 518 times
